Overview
Millions of individuals worldwide suffer from the widespread and complicated ailment known as chronic pain, which has a major negative influence on their everyday functioning and quality of life. In contrast to acute pain, which usually goes away over time, chronic pain lasts for several weeks, months, or even years, frequently surpassing the duration of the original disease or injury. An interdisciplinary strategy that takes into account the social, emotional, and physical components of chronic pain management is necessary. The symptoms, available treatments, and difficulties of dealing with chronic pain are examined in this article, which highlights the value of comprehensive care and continuous support for people with chronic discomfort.
Being Aware of Chronic Pain
Pain that lasts for three months or more—beyond the typical recovery period from an injury or illness—is classified as chronic pain. Numerous underlying ailments, including musculoskeletal disorders (like fibromyalgia or arthritis), nerve injury (neuropathic pain), or chronic illnesses (like diabetes or cancer) can cause it. A dull, aching, burning, or stabbing sensation might be the appearance of chronic pain, which can be localized in some parts of the body or pervasive. In contrast to acute pain, which acts as a defense mechanism, chronic pain frequently has no apparent physiological function and can have a major negative impact on daily activities and general health.
Difficulties in the Management of Chronic Pain
The management of chronic pain presents notable obstacles for both patients and healthcare professionals. These include the intricacies of identifying and treating underlying medical conditions, striking a balance between medication side effects and potential risks, and addressing the psychological and social aspects of pain relief. The stigma associated with the opioid crisis and chronic pain have also raised questions about access to adequate pain management treatments and complicated the care of those who are suffering from it. Optimizing pain treatment results for marginalized communities can also be hampered by healthcare inequities, inadequate insurance coverage, and restricted access to specialized pain management services.
Methods of Treating Chronic Pain
A thorough approach to treatment that is customized to each patient’s needs, preferences, and treatment objectives is necessary for managing chronic pain. Medications such as acetaminophen, nonsteroidal anti-inflammatory medicines (NSAIDs), antidepressants, anticonvulsants, or opioid analgesics are among the conventional therapy options for chronic pain. The goals of physical therapy methods, such as exercise, manual therapy, and heat or cold therapy, are to lessen pain severity while increasing function, strength, and mobility. When conservative therapy fail to relieve a particular pain issue, interventional procedures like nerve blocks, epidural injections, or spinal cord stimulation may be suggested.
The Signs and Effects of Persistent Pain
Beyond only physical suffering, chronic pain can have a wide range of negative effects on one’s body, mind, and social life. Fatigue, sleep difficulties, emotional swings (such as agitation, worry, or melancholy), and cognitive deficits (such trouble focusing or making decisions) can all result from persistent pain. In addition to interfering with relationships, employment, and leisure pursuits, chronic pain can also result in social isolation, financial hardship, and a lower standard of living. The ongoing load of pain can worsen resilience, hope, and self-worth, which exacerbates the effects on people who are living with chronic pain.
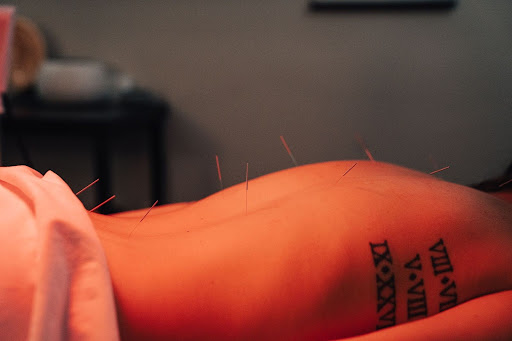
Holistic Methods for Treating Chronic Pain
Recognizing the interdependence of the mind, body, and spirit, holistic approaches to chronic pain management focus on the social, emotional, and physical elements of pain. Complementary therapies like acupuncture, massage therapy, yoga, tai chi, and mindfulness-based practices are frequently included in integrative pain management programs in order to improve physical functioning, relieve pain, and enhance overall well-being. Psychological therapies that assist people in developing coping mechanisms, lowering pain-related distress, and improving resilience in managing chronic pain include cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), and mindfulness-based stress reduction (MBSR).
Coping and Self-Management Techniques
Encouraging people to take an active role in managing their pain is crucial in fostering self-efficacy, autonomy, and overall wellbeing. Pacing activities, using relaxation techniques, leading a healthy lifestyle (consisting of regular exercise, a balanced diet, and enough sleep), and enlisting the help of friends, family, or support groups are some self-management options for chronic pain. In order to navigate the difficulties of living with chronic pain, mindfulness exercises, journaling, and creative activities like painting or music therapy can also offer channels for self-expression, stress reduction, and emotional healing.
Lobbying and Community Assistance
Raising awareness, lowering stigma, and promoting better access to all-encompassing pain management options for those with chronic pain are all made possible by advocacy and community support. Patient advocacy groups, internet discussion boards, and grassroots projects give people the chance to interact with others going through comparable difficulties, exchange stories, and gain access to tools and support systems. Communities may promote more understanding, compassion, and support for those facing long-term discomfort by elevating the voices of those with chronic pain and pushing for legislative changes that prioritize equitable access to efficient pain management solutions.
In summary
The complex and difficult experience of having chronic pain necessitates a thorough, interdisciplinary approach to management and care. Healthcare professionals can create individualized treatment programs that address the physical, emotional, and social components of chronic pain by having a thorough grasp of the symptoms, available treatments, and associated challenges. Integrative therapies, self-management techniques, and community support are examples of holistic approaches to chronic pain care that enable people to take an active role in their pain management and enhance general wellbeing. Communities may cooperate to lessen stigma, increase accessibility to efficient pain management treatments, and assist those who are experiencing chronic pain in their quest for healing and recovery through advocacy, education, and teamwork.